 |
|
 |
|
|
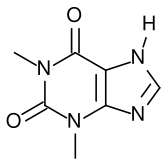
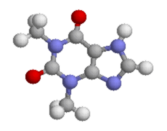
Theophylline
|
|
| Systematic (IUPAC) name | |
| 1,3-dimethyl-7H-purine-2,6-dione | |
| Identifiers | |
| CAS number | 58-55-9 |
| ATC code | R03DA04 |
| PubChem | 2153 |
| DrugBank | APRD00082 |
| Chemical data | |
| Formula | C7H8N4O2 |
| Mol. weight | 180.164 g/mol |
| Pharmacokinetic data | |
| Bioavailability | 100% |
| Protein binding | 40%, primarily to albumin |
| Metabolism | hepatic to 1-methyluric acid |
| Half life | 8 hours |
| Therapeutic considerations | |
| Pregnancy cat. | A(AU) C(US) |
| Legal status | P(UK) |
| Routes | oral, IV |
Theophylline is a methylxanthine drug used in therapy for respiratory diseases such as COPD or asthma under a variety of brand names. As a member of the xanthine family, it bears structural and pharmacological similarity to caffeine. It is naturally found in black tea and green tea.
The main actions of theophylline are:
- relaxing of bronchial smooth muscle
positive inotropic (increasing heart muscle contractility and efficiency)
positive chronotropic (increasing heart rate)
increase of blood pressure
increase of renal blood flow
some anti-inflammatory effects
History
Theophylline was first extracted from tea leaves around 1888 by the German biologist Albrecht Kossel. The drug was chemically identified in 1896 and eventually it was synthesized by another German scientist, Wilhelm Traube. Theophylline's first clinical use in asthma came in the 1950s.
Side effects
The use of theophylline is complicated by the fact that it interacts with various drugs, chiefly cimetidine and phenytoin, and that it has a narrow therapeutic index, so its use must be monitored to avoid toxicity. It can also cause nausea, diarrhea, increase in heart rate, arrhythmias and CNS excitation. Its toxicity is increased by erythromycin, cimetidine and fluoroquinolones.
The main therapeutic uses of theophylline are:
- chronic obstructive diseases of the airways
- chronic obstructive pulmonary disease (COPD)
- bronchial asthma.
A proposed mechanism of action includes a non-specific inhibition of phosphodiesterase enzymes, producing an increase in intracellular cyclic AMP; however, this is not known with certainty.[1][2][3]
Theophylline has been shown to inhibit TGF-beta mediated conversion of pulmonary fibroblasts into myofibroblasts in COPD and asthma via cAMP-PKA pathway and suppresses COL1 mRNA which codes for the protein collagen. (Yano, Biochem and Biophys Res Comm V341-3, 2006)
It has been shown that theophylline may reverse the clinical observations of steroid insensitivity in patients with COPD and asthmatics who are active smokers (a condition resulting in oxidative stress) via a distinctly separate mechanism. Theophylline in vitro can restore the reduced HDAC (histone deacetylase) activity that is induced by oxidative stress (i.e. in smokers), returning steroid responsiveness toward normal (Ito et al., 2002a). Furthermore, theophylline has been shown to directly activate HDAC2 (Ito et al., 2002b). (Corticosteroids switch off the inflammatory response by blocking the expression of inflammatory mediators through deacetylation of histones, an effect mediated via histone deacetylase-2 (HDAC2). Once deacetylated, DNA is rewound around histones and repackaged so that the promoter regions of inflammatory genes are unavailable for binding of transcription factors such as NFB that act to turn on inflammatory activity. It has recently been shown that the oxidative stress associated with cigarette smoke can inhibit the activity of HDAC2, thereby blocking the anti-inflammatory effects of corticosteroids.) Thus theophylline could prove to be a novel form of adjunct therapy in improving the clinical response to steroids in smoking asthmatics.




 216.73.216.133
216.73.216.133 User Stats:
User Stats:
 Today: 0
Today: 0 Yesterday: 0
Yesterday: 0 This Month: 0
This Month: 0 This Year: 0
This Year: 0 Total Users: 117
Total Users: 117 New Members:
New Members:
 216.73.xxx.xxx
216.73.xxx.xxx
 Server Time:
Server Time: