 |
|
|
Digoxin
|
|
| Systematic (IUPAC) name | |
|
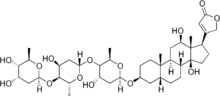
4-[(3S,5R,8R,9S,10S,12R,13S,14S)-3- [(2S,4S,5R,6R)-5-[(2S,4S,5R,6R)-5- [(2S,4S,5R,6R)-4,5-dihydroxy-6-methyl- oxan-2-yl]oxy-4-hydroxy-6-methyl-oxan- 2-yl]oxy-4-hydroxy-6-methyl-oxan-2-yl] oxy-12,14-dihydroxy-10,13-dimethyl-1, 2,3,4,5,6,7,8,9,11,12,15,16,17-tetra decahydrocyclopenta[a]phenanthren- 17-yl]-5H-furan-2-one |
|
| Identifiers | |
| CAS number | 20830-75-5 |
| ATC code | C01AA02 C01AA05 C01AA08 |
| PubChem | 30322 |
| DrugBank | APRD00098 |
| Chemical data | |
| Formula | C41H64O14 |
| Mol. weight | 780.938 g/mol |
| Pharmacokinetic data | |
| Bioavailability | 60 to 80% (Oral) |
| Protein binding | 25% |
| Metabolism | Hepatic (16%) |
| Half life | 36 to 48 hours (patients with normal renal function) 3.5 to 5 days (patients with impaired renal function) |
| Excretion | Urinary |
| Therapeutic considerations | |
| Pregnancy cat. | A (Au), C (U.S.) |
| Legal status | S4 (Au), POM (UK), ℞-only (U.S.) |
| Routes | Oral, Intravenous |
Digoxin (INN) (IPA: [dɪˈdʒɒksɪn]) is a cardiac glycoside extracted from the foxglove plant, digitalis. Its corresponding aglycone is digoxigenin. Digoxin is widely used in the treatment of various heart conditions, namely atrial fibrillation, atrial flutter and congestive heart failure that cannot be controlled by other medication. Digoxin preparations are commonly marketed under the trade name Lanoxin.
Contents |
Actions
The main pharmacological effects of digoxin are on the heart. Extracardiac effects are responsible for many of the adverse effects (see below).
Its main cardiac effects are
- A decrease of conduction of electrical impulses through the AV node, making it a commonly used drug in controlling the heart rate during atrial fibrillation or atrial flutter.
- An increase of force of contraction via inhibition of the Na+/K+ ATPase pump (see below).
Mechanism of action
Digoxin binds to a site on the extracellular aspect of the α-subunit of the Na+/K+ ATPase pump in the membranes of heart cells (myocytes). This causes an increase in the level of sodium ions in the myocytes, which then leads to a rise in the level of calcium ions. The proposed mechanism is the following: inhibition of the Na+/K+ pump leads to increased Na+ levels, which in turn slows down the extrusion of Ca2+ via the Na+/Ca2+ exchange pump. Increased amounts of Ca2+ are then stored in the sarcoplasmic reticulum and released by each action potential, which is unchanged by digoxin. This is a different mechanism from that of catecholamines.
Digoxin also increases vagal activity via its central action on the central nervous system, thus decreasing the conduction of electrical impulses through the AV node. This is important for its clinical use in different arrhythmias (see below).
Clinical use
Today, the most common indications for digoxin are probably atrial fibrillation and atrial flutter with rapid ventricular response. High ventricular rate leads to insufficient diastolic filling time. By slowing down the conduction in the AV node and increasing its refractory period, digoxin can reduce the ventricular rate. The arrhythmia itself is not affected, but the pumping function of the heart improves owing to improved filling.
The use of digoxin in congestive heart failure during sinus rhythm is controversial. In theory the increased force of contraction should lead to improved pumping function of the heart, but its effect on prognosis is disputable and digoxin is no longer the first choice for congestive heart failure. However, it can still be useful in patients who remain symptomatic despite proper diuretic and ACE inhibitor treatment.
Digoxin is usually given by mouth, but can also be given by IV injection in urgent situations (the IV injection should be slow, heart rhythm should be monitored). The half life is about 36 hours, digoxin is given once daily, usually in 125 μg or 250 μg dosing. In patients with decreased kidney function the half life is considerably longer, calling for a reduction in dosing or a switch to a different glycoside (such as digitoxin which although having a much longer elimination half-life of around 7 days, is mainly eliminated from the body via the liver, and thus not affected by changes in renal function).
Effective plasma levels are fairly well defined, 1-2.6 nmol/l. In suspected toxicity or ineffectiveness, digoxin levels should be monitored. Plasma potassium levels also need to be closely controlled (see side effects below).
Adverse effects
The occurrence of adverse drug reactions is common, owing to its narrow therapeutic index (the margin between effectiveness and toxicity). Adverse effects are concentration-dependent, and are rare when plasma digoxin concentration is <0.8 μg/L. [1] They are also more common in patients with low potassium levels (hypokalemia), since digoxin normally competes with K+ ions for the same binding site on the Na+/K+ ATPase pump.
Common adverse effects (≥1% of patients) include: loss of appetite, nausea, vomiting, diarrhoea, blurred vision, visual disturbances (yellow-green halos), confusion, drowsiness, dizziness, nightmares, agitation, and/or depression. Less frequent adverse effects (0.1%–1%) include: acute psychosis, delirium, amnesia, shortened QRS complex, atrial or ventricular extrasystoles, paroxysmal atrial tachycardia with AV block, ventricular tachycardia or fibrillation, heart block [1] but when sytematically sought, the evidence for this is equivocal.[2]
The pharmacological actions of digoxin usually results in electrocardiogram (ECG) changes, including ST depression or T wave inversion, which do not indicate toxicity. PR interval prolongation, however, may be a sign of digoxin toxicity. Additionally, increased intracellular Ca2+ may cause a type of arrhythmia called bigeminy (coupled beats), eventually ventricular tachycardia or fibrillation. The combination of increased (atrial) arrhythmogenesis and inhibited atrio-ventricular conduction (for example paroxysmal atrial tachycardia with A-V block - so-called "PAT with block") is said to be pathognomonic (i.e. diagnostic) of digoxin toxicity.[3]
An often described but rarely seen adverse effect of digoxin is a disturbance of colour vision (mostly yellow and green colour) called xanthopsia.
Digoxin has an interaction with the antimalarial medication Hydroxychloroquine.
Other information
Digoxin has potentially dangerous interaction with verapamil, amiodarone and erythromycin.
In overdose, the usual supportive measures are needed. If arrhythmias prove troublesome, or malignant hyperkalaemia occurs (inexorably rising potassium level due to paralysis of the cell membrane bound ATPase-dependant Na/K pumps), the specific antidote is antidigoxin (antibody fragments against digoxin, trade name Digibind®). [4] Digoxin is not usefully removed by hemodialysis.
Some physical properties of digoxin are water solubility of 64.8 mg/L at 25 °C and melting point at 249.3 °C.
In the news
Charles Cullen admitted in 2003 to killing as many as 40 hospital patients with overdoses of heart medication - usually digoxin - at hospitals in New Jersey and Pennsylvania over his 16-year career as a nurse. On March 10, 2006 he was sentenced to 18 consecutive life sentences and is not eligible for parole for 397 years. [3]
See also
References
- ^ a b Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- ^ Drug-induced gynecomastia. Thompson DF, Carter JR. Pharmacotherapy. 1993 Jan-Feb;13(1):37-45. [1]
- ^ Digitalis intoxication: specifity and significance of cardiac and extracardiac symptoms. part I: Patients with digitalis-induced arrhythmias (author's transl). Doering W, Konig E, Sturm W. Z Kardiol. 1977 Mar;66(3):121-8. [2]
- ^ Fab antibody fragments: some applications in clinical toxicology. Flanagan RJ & Jones AL Drug Saf 2004;27(14):1115-33. PMID: 15554746 (accessed 19 Sep 2006)
Further reading
- Rang HP, Dale MM, Ritter JM, Moore PK. Pharmacology, 5th edition. Edinburgh: Churchill Livingstone; 2003. ISBN 0-443-07145-4
- Summary of product characteristics, Digoxin 0,125 mg, Zentiva a.s.
- Lüllmann. Pharmakologie und Toxikologie (15th edition), Georg Thieme Verlag, 2003. ISBN 3-13-368515-5




 216.73.216.2
216.73.216.2 User Stats:
User Stats:
 Today: 0
Today: 0 Yesterday: 0
Yesterday: 0 This Month: 0
This Month: 0 This Year: 0
This Year: 0 Total Users: 117
Total Users: 117 New Members:
New Members:
 216.73.xxx.x
216.73.xxx.x
 Server Time:
Server Time: