ACE inhibitors, or inhibitors of Angiotensin-Converting Enzyme, are a group of pharmaceuticals that are used primarily in treatment of hypertension and congestive heart failure, in most cases as the drugs of first choice.
Contents |
Clinical use
Indications for ACE inhibitors include:
- Prevention of cardiovascular disorders
Congestive heart failure
Hypertension
Left ventricular dysfunction
Prevention of nephropathy in diabetes mellitus
In several of these indications, ACE inhibitors are used first-line as several agents in the class have been clinically shown to be superior to other classes of drugs in the reduction of morbidity and mortality.
ACE inhibitors are often combined with diuretics in the control of hypertension (usually a thiazide), when an ACE inhibitor alone proves insufficient; and in chronic heart failure (usually furosemide) for improved symptomatic control. Thus there exists, on the market, combination products combining an ACE inhibitor with a thiazide (usually hydrochlorothiazide) in a single tablet to allow easy administration by patients.
Effects of ACE inhibitors
ACE inhibitors lower arteriolar resistance and increase venous capacitance; increase cardiac output and cardiac index, stroke work and volume, lower renovascular resistance, and lead to increased natriuresis (excretion of sodium in the urine).
Epidemiological and clinical studies have shown that ACE inhibitors reduce the progress of diabetic nephropathy independently from their blood pressure-lowering effect. This action of ACE inhibitors is utilised in the prevention of diabetic renal failure.
ACE inhibitors have been shown to be effective for indications other than hypertension even in patients with normal blood pressure. The use of a maximum dose of ACE inhibitors in such patients (including for prevention of diabetic nephropathy, congestive heart failure, prophylaxis of cardiovascular events) is justified because it improves clinical outcomes, independent of the blood pressure lowering effect of ACE inhibitors. Such therapy, of course, requires careful and gradual titration of the dose to prevent the patient suffering from the effects of rapidly decreasing their blood pressure (dizziness, fainting, etc).
Adverse effects
Common adverse drug reactions (≥1% of patients) include: hypotension, cough, hyperkalemia, headache, dizziness, fatigue, nausea, renal impairment.[1]
A persistent dry cough is a relatively common adverse effect believed to be associated with the increases in bradykinin levels produced by ACE inhibitors, although the role of bradykinin in producing these symptoms remains disputed by some authors.[2] Patients who experience this cough are often switched to angiotensin II receptor antagonists.
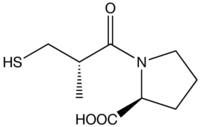
Rash and taste disturbances, infrequent with most ACE inhibitors, are more prevalent in captopril and is attributed to its sulfhydryl moiety. This has led to decreased use of captopril in clinical setting, although it is still used in scintigraphy of the kidney.
Renal impairment is a significant adverse effect of all ACE inhibitors, and is associated with their effect on angiotensin II-mediated homeostatic functions such as renal bloodflow. ACE inhibitors can induce or exacerbate renal impairment in patients with renal artery stenosis. This is especially a problem if the patient is also concomitantly taking an NSAID and a diuretic - the so-called "triple whammy" effect - such patients are at very high risk of developing renal failure. [3]
Some patients develop angioedema due to increased bradykinin levels. There appears to be a genetic predisposition towards this adverse effect in patients who degrade bradykinin slower than average.[4]
Examples of ACE inhibitors
ACE inhibitors can be divided into three groups based on their molecular structure:
Sulfhydryl-containing ACE inhibitors
- Captopril (Capoten®), the first ACE inhibitor
Dicarboxylate-containing ACE inhibitors
This is the largest group, including:
- Enalapril (Vasotec®/Renitec®)
Ramipril (Altace®/Tritace®/Ramace®)
Quinapril (Accupril®)
Perindopril (Coversyl®)
Lisinopril (Lisodur®/Lopril®/Prinivil®/Zestril®)
Benazepril
Phosphonate-containing ACE inhibitors
- Fosinopril (Monopril®), the only member
Naturally occurring
Casokinins and lactokinins are breakdown products of casein and whey that occur naturally after ingestion of milk products, especially sour milk. Their role in blood pressure control is uncertain.[5]
Comparative information
Comparatively, all ACE inhibitors have similar antihypertensive efficacy when equivalent doses are administered. The main point-of-difference lies with captopril, the first ACE inhibitor, which has a shorter duration of action and increased incidence of certain adverse effects (cf. captopril).
Certain agents in the ACE inhibitor class have been proven, in large clinical studies, to reduce mortality post-myocardial infarction, prevent development of heart failure, etc. While these effects are likely to be class-effects, good evidence-based medicine practice would direct the use of those agents with established clinical efficacy.
Contraindications and precautions
The ACE inhibitors are contraindicated in patients with:
- Previous angioedema associated with ACE inhibitor
therapy
Renal artery stenosis (bilateral, or unilateral with a solitary functioning kidney)
ACE inhibitors should be used with caution in patients with:
- Impaired renal function
Aortic valve stenosis or cardiac outflow obstruction
Hypovolaemia or dehydration
Haemodialysis with high flux polyacrylonitrile membranes
ACE inhibitors are ADEC Pregnancy category D, and should be avoided in women who are likely to become pregnant.[1] In the U.S., ACE inhibitors are required to be labelled with a "black box" warning concerning the risk of birth defects when taking during the second and third trimester. It has also been found that use of ACE inhibitors in the first trimester is also associated with a risk of major congenital malformations, particularly affecting the cardiovascular and central nervous systems.[6]
Potassium supplementation should be used with caution and under medical supervision owing to the hyperkalaemic effect of ACE inhibitors.
Angiotensin II receptor antagonists
ACE inhibitors share many common characteristics with another class of cardiovascular drugs called angiotensin II receptor antagonists, which are often used when patients are intolerant of the adverse effects produced by ACE inhibitors. ACE inhibitors do not completely prevent the formation of angiotensin II, as there are other conversion pathways, and so angiotensin II receptor antagonists may be useful because they act to prevent the action of angiotensin II at the AT1 receptor.
Use in combination with ACE inhibitors
While counterintuitive at first glance, the combination therapy of angiotensin II receptor antagonists with ACE inhibitors may be superior to either agent alone. This combination may increase levels of bradykinin while blocking the generation of angiotensin II and its activity at the AT1 receptor. This 'dual blockade' may be more effective than using an ACE inhibitor alone, because angiotensin II can be generated via non-ACE-dependent pathways. Preliminary studies suggest that this combination of pharmacologic agents may be advantageous in the treatment of essential hypertension, chronic heart failure, and nephropathy.[7][8] However, more studies are needed to confirm these highly preliminary results. While statistically significant results have been obtained for its role in treating hypertension, clinical significance may be lacking.[9]
Patients with heart failure may benefit from the combination in terms of reducing morbidity and ventricular remodeling.[10][11]
The most compelling evidence has been found for the treatment of nephropathy: this combination therapy partially reversed the proteinuria and also exhibited a renoprotective effect in patients afflicted with diabetic nephropathy, (Luno et al., 2005) and pediatric IgA nephropathy.[12]
History
The first step in the development of ACE inhibitors was the discovery of angiotensin converting enzyme (ACE) in 1956 by Leonard T. Skeggs. The importance of this enzyme in blood pressure regulation was initially underestimated. Fourteen years later, the pharmacologist Sérgio Henrique Ferreira discovered that the venom of the pit viper (Bothrops jararaca) was able to potentiate the action of bradykinin. A family of peptides, designated bradykinin potentiating factors (BPFs) was isolated from the venom and their action was linked to inhibition of bradykinin degradation by ACE.
The nonapeptide BPF teprotide (SQ 20,881) was found to have the greatest ACE inhibition potency and hypotensive effect in vivo. Teprotide had limited clinical value, however, due to its peptide nature and lack of activity when given orally. In the early 1970s, knowledge of the structure-activity relationship required for inhibition of ACE was growing. David Cushman, Miguel Ondetti and colleagues used peptide analogues to study the structure of ACE, using carboxypeptidase A as a model. Their discoveries led to the development of captopril, the first orally-active ACE inhibitor, in 1975.
Captopril was approved by the United States Food and Drug Administration in 1981. The first non-sulfhydryl-containing ACE inhibitor enalapril was marketed two years later. Since then, at least nine other ACE inhibitors have been marketed.
References
- ^ a b Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3.
- ^ Okumura H, Nishimura E, Kariya S, et al. Angiotensin-converting enzyme (ACE) 阻害薬誘発性の咳嗽発現とACE遺伝子型,血漿中ブラジキニン,サブスタンスP及びACE阻害薬濃度との関連性 [No relation between angiotensin-converting enzyme (ACE) inhibitor-induced cough and ACE gene polymorphism, plasma bradykinin, substance P and ACE inhibitor concentration in Japanese patients]. Yakugaku Zasshi 2001;121(3):253-7. Japanese. PMID 11265121
- ^ Thomas MC. Diuretics, ACE inhibitors and NSAIDs - the triple whammy. Med J Aust 2000;172(4):184–185. PMID 10772593
- ^ Molinaro G, Cugno M, Perez M, et al. Angiotensin-converting enzyme inhibitor-associated angioedema is characterized by a slower degradation of des-arginine(9)-bradykinin. J Pharmacol Exp Ther 2002;303:232-7. PMID 12235256.
- ^ FitzGerald RJ, Murray BA, Walsh DJ. Hypotensive peptides from milk proteins. J Nutr 2004;134:980S-8S. PMID 15051858.
- ^ Cooper WO, Hernandez-Diaz S, Arbogast PG, Dudley JA, Dyer S, Gideon PS, et al. Major congenital malformations after first-trimester exposure to ACE inhibitors. N Engl J Med 2006;354(23):2443-51. PMID 16760444
- ^ Luno J, Praga M, de Vinuesa SG. The reno-protective effect of the dual blockade of the renin angiotensin system (RAS). Curr Pharm Des 2005;11(10):1291-300. PMID 15853685
- ^ van de Wal RM, van Veldhuisen DJ, van Gilst WH, Voors AA. Addition of an angiotensin receptor blocker to full-dose ACE-inhibition: controversial or common sense? Eur Heart J 2005;26(22):2361-7. PMID 16105846
- ^ Finnegan PM, Gleason BL. Combination ACE inhibitors and angiotensin II receptor blockers for hypertension. Ann Pharmacother 2003;37(6):886-9. PMID 12773079
- ^ Krum H, Carson P, Farsang C, et al. Effect of valsartan added to background ACE inhibitor therapy in patients with heart failure: results from Val-HeFT. Eur J Heart Fail 2004;6(7):937-45. PMID 15556056
- ^ Solomon SD, Skali H, Anavekar NS, et al. Changes in ventricular size and function in patients treated with valsartan, captopril, or both after myocardial infarction. Circulation 2005;111(25):3411-9. PMID 15967846
- ^ Yang Y, Ohta K, Shimizu M, et al. Treatment with low-dose angiotensin-converting enzyme inhibitor (ACEI) plus angiotensin II receptor blocker (ARB) in pediatric patients with IgA nephropathy. Clin Nephrol 2005;64(1):35-40. PMID 16047643




 216.73.216.133
216.73.216.133 User Stats:
User Stats:
 Today: 0
Today: 0 Yesterday: 0
Yesterday: 0 This Month: 0
This Month: 0 This Year: 0
This Year: 0 Total Users: 117
Total Users: 117 New Members:
New Members:
 216.73.xxx.xxx
216.73.xxx.xxx
 Server Time:
Server Time: